Multidrug resistant bacteria or “super bugs” are emerging rapidly nowadays causing deadly infections becuase of ineffectiveness of available antimicrobials or treatment options.
World Health Organization

Multidrug Resistant or Extended-Spectrum Beta-Lactamase (ESBL)–Producing Bacteria
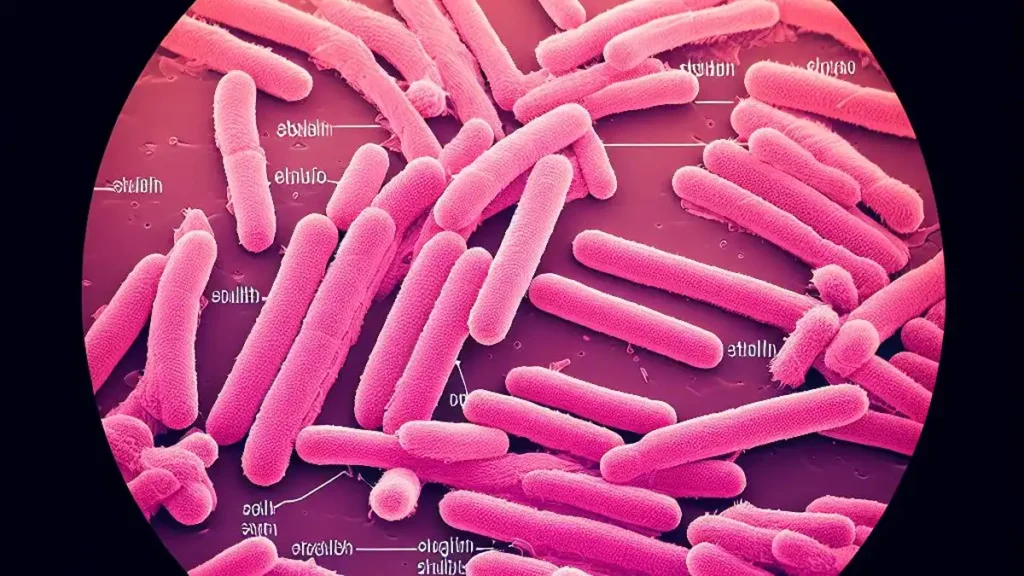
Firstly, ESBL producing gram negative species of bacteria especially Enterobacteriaceae are identified to possess acquired resistance against beta-lactam antibiotics by production of enzymes called “beta-lactamase”. These enzymes inactivate beta-lactam antibiotics by hydrolyzing its beta-lactam ring found in the drug structure. Penicillinase was the first beta-lactamase isolated in E coli in 1940, before therapeutic use of penicillin drug.
New antibiotics developed to resist the effects of beta-lactamase include broad-spectrum cephalosporins which further lead to antibiotic resistance against broader-spectrum antibiotics. Currently, there are >150 ESBLs found in P aeruginosa and Enterobacteriaceae species causing serious infections. ESBL producing Enterobacteriaceae is included in first priority published by World Health Organization priority pathogens list (Priority 1:critical list ) which urges the need of Research & Development of new antibiotics.
Multidrug Resistant Bacteria or Carbapenems resistance?
Secondly, carbapenem resistance is also emerging rapidly nowadays especially in Enterobacteriaceae genus. Carbapenem drug is the subgroup of beta-lactam antibiotics including meropenem, ertapenem, doripenem, and imipenem. Carbapenems are the broadest spectrum antibiotics available and have been the drug of choice for ESBL-producing bacteria and gram-negative nosocomial infections. Similar to ESBL enzymes, produced by selective pressure of broad-spectrum cephalosporins, carbapenem-resistant emerge by use of carbapenem drugs by production of carbapenemase enzyme in carbapenem-resistant bacteria making them capable of hydrolysing carbapenem ring.
Therefore, increase in carbapenem-resistant bacteria is due to carbapenem drug overuse. Carbapenem-resistant Enterobacteriaceae (CRE) and Acinetobacter are linked to combined hospitalization of twenty one thousand six hundred (21,600) patients and eighteen hundred (1,800) deaths annually in United States. Other bacteria which may develop carbapenem resistance include K pneumoniae, P aeruginosa, and E coli. Carbapenemase producing Enterobacteriaceae is also included in first priority (Priority 1: CRITICAL) published by World Health Organization priority pathogens list which urges the need of Research & Development of new antibiotics.
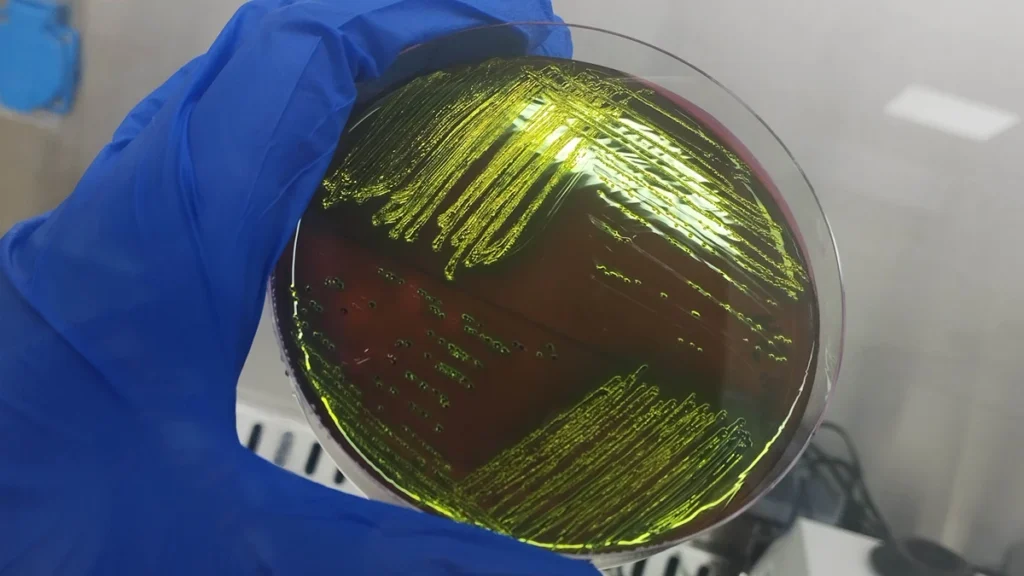
Multidrug Resistant Enterobacteriaceae and ampC producers
Thirdly, AmpC producing Enterobacteriaceae is also included in first priority critical pathogen list published by World Health Organization which urges the need of Research & Development of new antibiotics. There are more than 100 species of Enterobacteriaceae but a few (Serratia marcescens, Morganella morganii, Proteus vulgaris, Citrobacter species, and Enterobacter species) have an inducible beta-lactamase enzyme known as ampC. The ampC enzyme is not expressed normally in culture sensitivity test in laboratory but it may be deceiving.
However, several penicillins and 1st to 3rd generation cephalosporins do not show drug resistance but these drugs activate ampC enzyme and will induce antibiotic resistance. AmpC enzyme can be detected in antibiotic sensitivity testing if bacteria is resistant to cefoxitin phenotypically this may serve as a surrogate marker for ampC. So in this case penicillins and narrow-spectrum cephalosporins should not be prescribed.
Rapidly Emerging Colistin resistance
Fourthly, Colistin resistance is also crucial because it is the last available drug choices left with humanity in complicated infections. Colistin belongs to polymyxins group of antimicrobial, originally isolated from Paenibacillus polymyxa, the spore-forming soil organism. Members of this group include polymyxins A, B, C, D and E, of which only polymyxin E (colistin) and polymyxin B are clinically used in humans. Moreover, Colistin is used clinically in both human and veterinary medicine to treat infections.
Hence, with the emergence of MDR bacteria and carbapenemase-producing Enterobacteriaceae colistin has been considered as last resort for treatment of resistant bacteria therefore, the emergence of colistin resistance in multidrug-resistant bacteria is significant clinically and it is a serious public health concern. Bacteria alter Gram-negative outer membrane lipopolysaccharides through mutations in mgrB gene. However, plasmid mediated emergence of colistin resistance recently among Enterobacteriaceae poses a serious threat to global public health.
Multidrug Resistant Enterococcus
Fifthly, multidrug resistant Enterococcus specie is also very important also included in second priority of highly important pathogen list published by World Health Organization which urges the need of Research & Development of new antibiotics. Enterococcus genus is predominantly a gut bacteria used as indicator bacteria equipped with intrinsic and acquired antibiotic resistance. Enterococcus faecium and Enterococcus faecalis species are of special importance. Enterococcus can have multiple acquired resistance mechanisms therefore result in multidrug resistant bacteria. High levels of resistance may exist in Enterococcus including
- Beta-lactams resistant Enterococcus (through beta-lactamase enzymes and altered binding proteins),
- Vancomycin resistant Enterococcus (via changes in peptidoglycan synthesis; known as VRE), and
- Aminoglycosides resistant Enterococcus (through enzymatic degradation).
Ampicillin is the drug of choice for susceptible Enterococcus infections but few options including linezolid, daptomycin, and tigecycline can also be considered for MDR Enterococcus infections.

Methicillin-Resistant Staphylococcus aureus (MRSA) and mecA
Sixthly, methicillin-resistant Staphylococcus aureus and vancomycin-intermediate and resistant staphylococcus aureus are also included in second priority of highly important pathogen list published by World Health Organization which urges the need of Research & Development of new antibiotics. MRSA was first recovered in early 1960s after the discovery of methicillin.
In gram-positive bacteria cell wall is the main target site for antimicrobial drugs and bacteria alters its cell wall to confer antibiotic resistance. Methicillin-resistant Staphylococcus aureus must possess mecA gene which encodes for a structural change in penicillin-binding protein 2a (PBP2a).This altered binding site prevents beta-lactam antibiotics from binding to the cell wall.
However, Methicillin-resistant Staphylococcus aureus susceptibility is not determined against methicillin to the instability of methicillin plates rather it is determined by oxacillin, a similar beta-lactam for confirmation in laboratory through Antibiotic sensitivity testing. The Clinical Laboratory Standards Institute defines methicillin resistance as an oxacillin which means isolates resistant to oxacillin with inhibitory concentration of at least 4 mcg/mL are resistant to all beta-lactams.

