Key facts
Sustainable Development Goals (SDGs)
Antimicrobial resistance (AMR) requires urgent multi-sectoral actions to achieve sustainable development goals (SDGs).
Health Emergency
World Health Organization has declared that AMR is one of the top 10 global public health threats facing humanity.
Financial Crisis
Cost of AMR is is significant on the economy due to prolonged illness , need of expensive medicine, disability and death.
Why is Antimicrobial Resistance (AMR) Important?
AMR is also a major public health and one health concern globally due to emergence, transmission and persistence of multidrug resistant (MDR) microbes in recent years across humans, animals, plants and the environment. Currently, at least 700,000 people die each year due to drug-resistant diseases according to report of the UN Ad hoc Interagency Coordinating Group on Antimicrobial Resistance and it is expected to up to 10 million deaths each year by 2050 and damage to the economy as catastrophic as the 2008-2009 global financial crisis if not given attention to prevent spread of drug resistance bacteria. By 2030, antimicrobial resistance could force up to 24 million people into extreme poverty.
What is Antimicrobial Resistance (AMR)?
Antimicrobial resistance is a phenomenon that occurs in microbes when they develop a defense mechanism against drugs which are designed to kill them. It occurs when microbes like bacteria, viruses, fungi and parasites change their genetic makeup through mutation or acquire resistance genes.
- Real world – clinical definition: Resistance is the ability of a bacterial strain to survive or grow during antimicrobial treatment
- Research – genetic definition: Resistance is defined by the presence of a genetic change (mutation or gene) = resistance determinant
- Laboratory – microbiological definition: Resistance is the ability to survive or grow in higher antibiotic concentrations than most other bacterial strains of the same species
How Bacteria Develop Drug Resistance?
In order to develop antimicrobial resistance bacteria adopts various mechanisms to make antibiotic ineffective for example they produce enzymes to degrade antimicrobials, alter proteins that are the binding sites for drugs or change membrane permeability to avoid influx of antibiotics and develop efflux pumps to pump out antimicrobials outside the bacteria.
As a result of drug resistance, microbes (bacteria) no longer respond to available antibiotics, making them ineffective which makes infections harder or impossible to treat due to antibiotic resistant bacteria and it also increases the risk of disease spread, severe illness and death. As a result of emerging antibiotic resistance in bacteria there is a looming threat of multidrug resistant also called MDR or extensively drug resistant/ extremely drug resistant bacteria also called XDR outbreaks in hospitals and community which is a serious concern for public health.
How Antimicrobial Resistance Spread?
Antimicrobial resistance is a one health issue because it includes all the sectors including human health, animal health agriculture, fisheries and environment. AMR develops in organisms like bacteria found in people, animals, food, plants and the environment (in water, soil and air) due to overuse or misuse of drugs like antibiotics. These resistant bacteria can spread among humans, between humans and animals through food of animal origin and between humans and plants through food of plant origin.
Currently there are few new antibiotic drugs in drug discovery pipeline and we only have few available drugs for treatment options particularly for gram negative bacteria while rapid global spread of multi- and pan-resistant bacteria (also known as “superbugs”) is alarming because infections caused by these organisms (bacteria) are not treatable with currently available antimicrobials e.g. antibiotics. Therefore, all stakeholders must join hands through multi-sectoral collaboration to control this issue.

What are the main drivers of AMR spread?
Main drivers in spread of AMR include,
- Misuse and overuse of antimicrobials in humans, animals and plants
- Lack of access to clean water
- Poor sanitation and hygiene (WASH) for both humans and animals
- Poor infection and disease prevention and control in health-care facilities and farms
- Lack of access to quality, affordable medicines, vaccines and diagnostics
- Lack of awareness and knowledge and
- Lack of appropriate legislation and lack implementation of existing legislation.
How Antibiotic Resistance is Burden on Economy?
Antimicrobial resistance particularly antibacterial resistance puts significant burden on national economies and health systems of countries as it affects patient’s health and their families through prolonged health expenses and stay in hospitals and the need of expensive drugs. Therefore, it is a major threat to countries with high population and poor economies having poor health systems.
What is the Effect of Antibiotic Resistance?
Fate of available treatment options
With the passage of time, available antibiotics are becoming ineffective which is making infections difficult or impossible to treat leading to severe illness, disability and deaths. It urgently requires discovery of new antibiotics or drugs otherwise available drugs will become ineffective as well e.g. tuberculosis antimicrobial resistance and MDR TB or carbapenem resistant E.coli in humans. However, with judicial use antibiotics in humans, animals and plants drug resistance can be controlled to avoid catastrophic situation in global health system.
How to prevent Antimicrobial Resistance (AMR)?
- Scientific knowledge and science-based evidence are needed to identify, manage and mitigate AMR risks before they become large-scale emergencies.
- Good husbandry practices, biosecurity, sanitation, hygiene, vaccination and other infection prevention measures are essential to reduce the need for antimicrobials in animals and antimicrobial pesticides in plants.
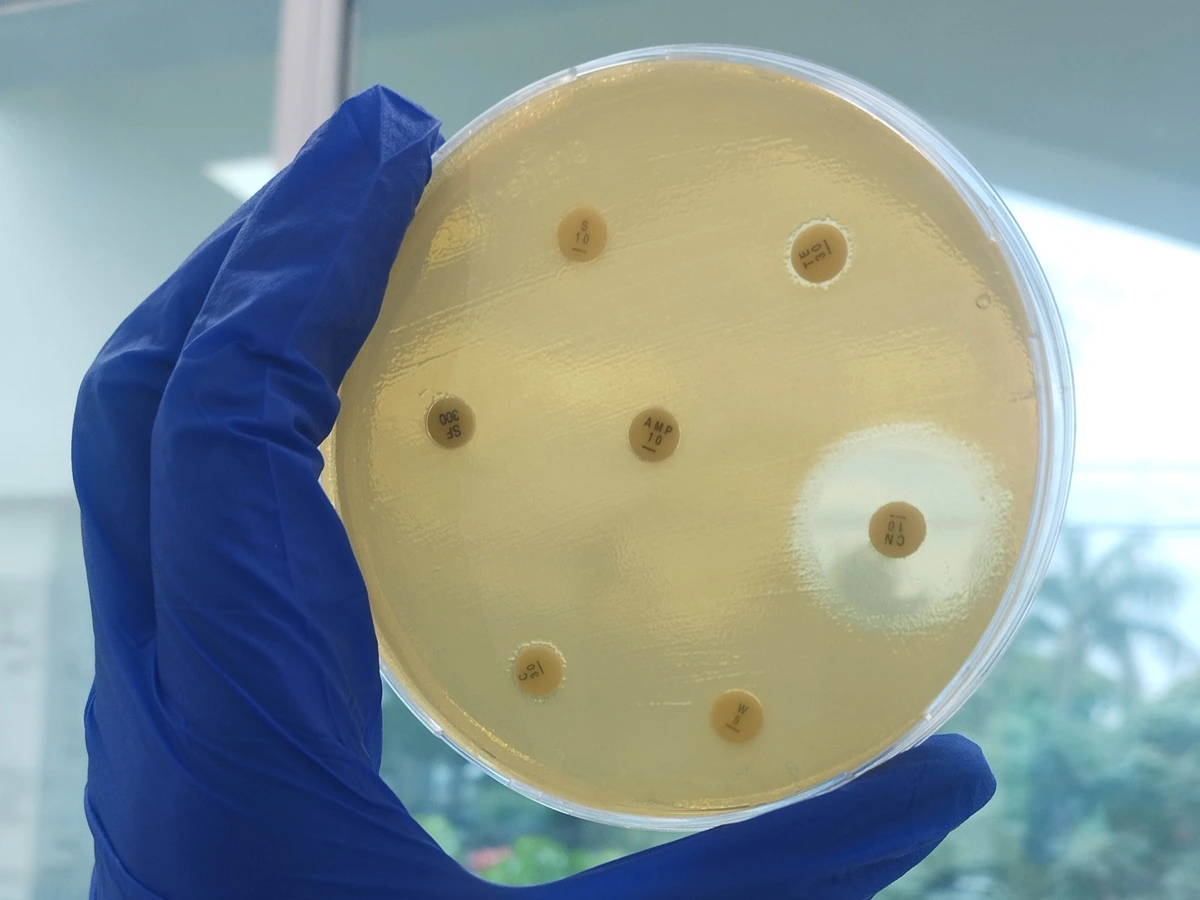
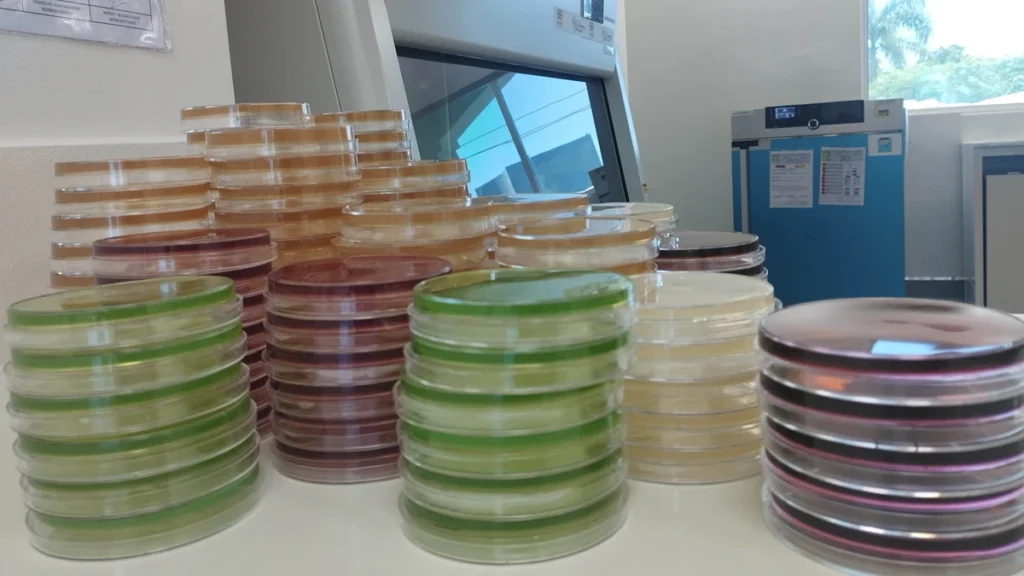
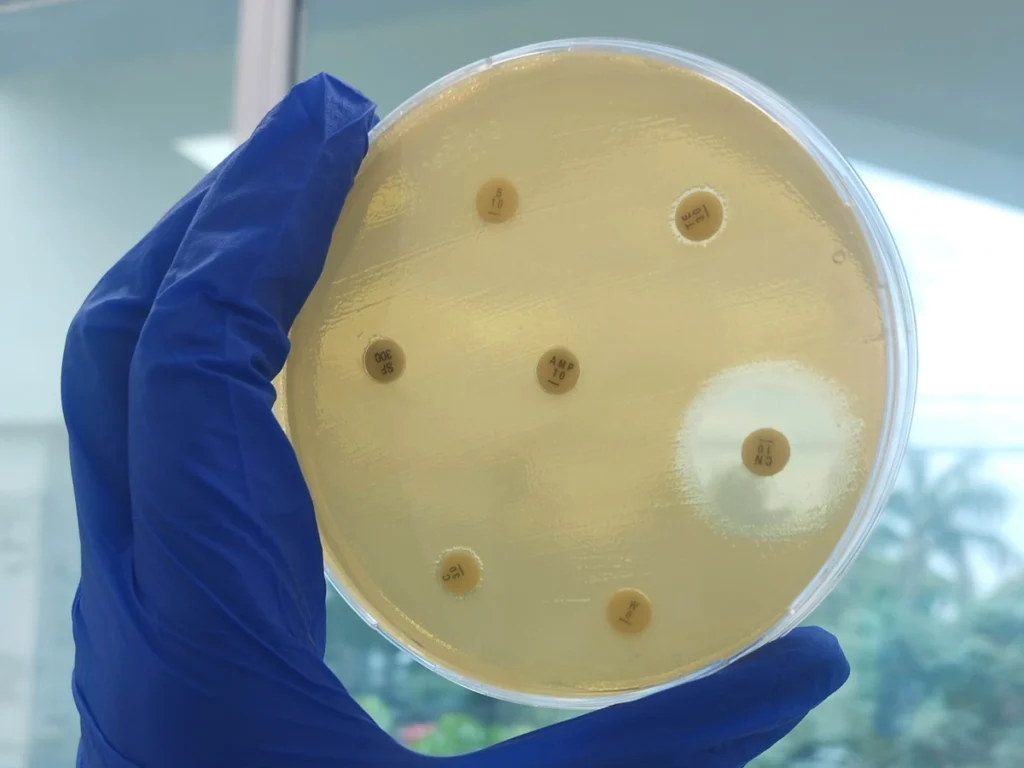
- Laboratory diagnostic and sensitivity tests are essential for the detection of AMR. They guide therapeutic treatments to save human and animal lives. They also play a key role in surveillance efforts to design successful interventions to reduce AMR in humans, animals, plants and the environment.
- Improving access to expert advice, prescriptions, appropriate antimicrobials will limit the development of AMR, reduce production and productivity losses and build more sustainable and resilient agrifood systems.
- The use of Integrated Pest Management and good agricultural practices provides a system-wide approach to keeping crops healthy, resorting to chemical pesticides, including antimicrobials, only as a last option.
- Good governance of AMR requires regulation of substandard and counterfeit antimicrobials and investment in reducing AMR at national level in line with the commitments of the Global Action Plan.
Fighting AMR is a true endeavor throughout the globe. It is a complex problem that requires a united multi-sectoral collaboration. The One Health approach brings together multiple sectors and stakeholders engaged in human, animal (terrestrial and aquatic animal), agriculture (food and feed production) and the environment to communicate and work together in the global action plan and implement policies, legislation and research to attain better public health outcomes.
To curb it effectively, all stakeholders must join forces and encourage the prudent use of antimicrobials, as well as preventive measures.