According to WHO annual analyses, in 2021 there were only 27 new antibiotics in clinical development against priority pathogens, down from 31 products in 2017.

After Antimicrobial drugs or antibiotic (Penicillin was the first drug discovered in 1928) by Alexander Fleming discovery of antibiotics (Penicillin was the first drug discovered in 1928 by Alexander Fleming), scientists believed that the war against infectious bacteria is over because it attributed to 70 percent decline in deaths due to infectious bacterial infections. With the passage of time microbes or bacteria evolved mechanisms to cope with antibiotic exposure through different routes which is called acquired resistance or resistance genes in bacterial genome. In addition to acquired resistance many bacteria are inherently resistant to available treatment options.
Rapid emergence of antimicrobial resistance phenomenon proved scientists wrong as antimicrobial resistant bacteria appeared as serious threat to humanity being responsible for at least 700,000 deaths/ year globally nowadays. Despite high death rate due to infectious diseases and the looming threat of antibiotic resistance, new drug discovery rate has declined over past 75 years and antimicrobial resistance has further worsened the impact of infectious diseases raising both incidence and cost of infections.
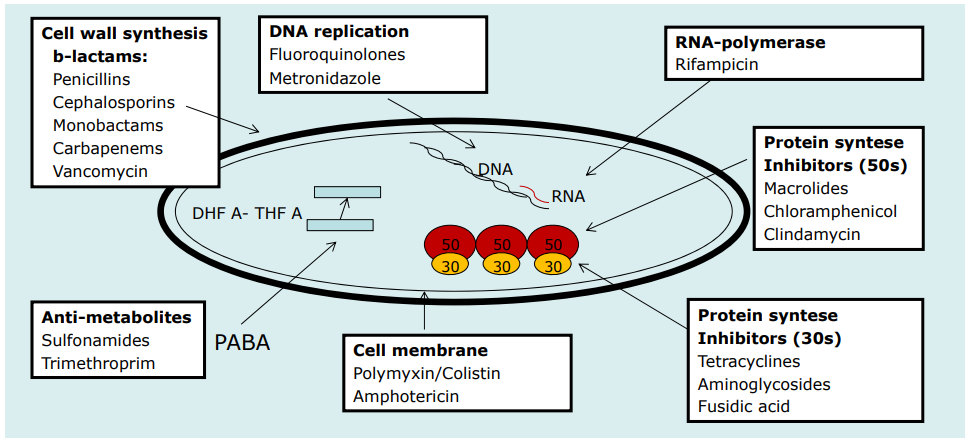
To understand the antimicrobial resistance it is important to understand available antimicrobial drugs for treatment of infectious bacterial diseases nowadays and how different antimicrobial drugs work to kill or inhibit bacteria by inhibiting the natural processes of bacterial cells. In this blog we will discuss different antimicrobial classes and their mode of actions to develop basis understanding about antimicrobial resistance.

Targets of antimicrobial action
Antimicrobial drugs generally target 5 different targets of bacteria to kill or inhibit it including Cell wall synthesis, protein synthesis, ribonucleic acid synthesis, deoxyribonucleic acid (DNA) synthesis, and intermediate metabolism. Discovery of new antimicrobial drugs and knowledge of existing antimicrobial drugs mechanisms of action is essential.
Modes of antimicrobial action
1. Inhibition of cell wall synthesis
Bacterial cell wall synthesis
Bacteria have a rigid cell wall composed of peptidoglycan which surrounds the cytoplasmic membrane and prevents osmotic lysis. It is composed of interlocking chains of building blocks called peptidoglycan monomers.
During bacterial replication through binary fission, bacteria have to synthesize new cell wall by synthesis of interlocking peptidoglycan molecules in the cytoplasm, transport them across the cytoplasmic membrane, breakdown previous cell wall for incorporation of new peptidoglycan monomers, bind them to the existing peptidoglycan, and develop cross-links between peptidoglycan layers.
Many antibiotics inhibit peptidoglycan synthesis in bacteria and lead to osmotic lysis of the bacteria. Antimicrobial drugs which inhibit cell wall synthesis in bacteria include
- Beta lactams
- bacitracin
- vancomycin
Gram positive/ Gram negative cell wall
Most bacteria can be placed into one of three groups based on their color after specific staining procedures are performed: Gram-positive, Gram-negative, or acid-fast. These staining reactions are due to fundamental differences in the bacterial cell wall. Gram-positive bacteria stain purple after Gram staining while Gram-negative bacteria stain pink.

2. Inhibition of DNA synthesis
Bacterial DNA replication
DNA replication is complex and multistep process in bacterial cell when it divides through binary fission. This process involves few steps including unwinding of DNA double helix and the synthesis of sister DNA strands using the parent DNA chain as a template and during this process, there are few essential enzymes that catalyse a series of reactions to make sure that high precision and complete replication per cell-division cycle. DNA gyrase (topoisomerase II) and topoisomerases (I and III) play important role in maintenance of structure and the compact supercoiled domains of the chromosome. These also help in the process of winding and unwinding of the DNA that occurs during replication and transcription.
Therefore, inhibiting DNA synthesis by blockage of these enzymes is an important therapeutic strategy by antimicrobial drugs including Quinolone drug class Inhibition of DNA-gyrase in microbe results in inhibition of ATP-dependent negative supercoiling of DNA, inhibition or ATP-independent relaxation of supercoiled DNA, and facilitation of double-stranded DNA breakage. Antimicrobial drugs which inhibit DNA synthesis in bacteria include
3. Inhibition of protein synthesis
Protein synthesis is a complex process including transcription and translation involving many enzymes which help in protein synthesis. Most of antibiotics which inhibit protein synthesis interfere with 30S subunit or 50S subunit of the 70S bacterial ribosome. Protein synthesis inhibitor antimicrobials mainly target three sites in the process of protein synthesis including
- Initiation complex formation (30S) including mRNA, 30S ribosomal subunit, and formyl-methionyl-transfer RNA)
- The formation of the 70S ribosome(by the 30S initiation complex and the 50S ribosome subunit) and
- Amino acid assembling into polypeptides called the elongation process
Antimicrobial drugs which inhibit or block protein synthesis include
4. Inhibition of folic acid synthesis
Bacterial cell is unable to absorb folic acid therefore, it needs to synthesize folic acid from PABA (para-aminobenzoic acid), pteridine, and glutamate. This pathway is selective target for antimicrobials for bacterial cell because humans cannot synthesize folic acid. Dihydropteroate synthetase and Dihydrofolate reductase are the two enzymes in folate pathway used by antimicrobials to inhibit or kill bacteria. Antimicrobial drugs which inhibit folate synthesis pathway include
5. Disruption of osmotic integrity
Antimicrobial drugs belonging to the family of polymyxins including colistin are mainly active against gram-negative organisms. They kill bacterial cell by changing the permeability of the cell wall by binding anionic lipopolysaccharide molecules and displacement of calcium and magnesium leading to cell leakage and death.
Antibiotic resistance against these antimicrobial drugs drugs is alarming because this group of drugs is considered last line of treatment in humans. Antimicrobial drugs involving disruption of cell wall integrity include