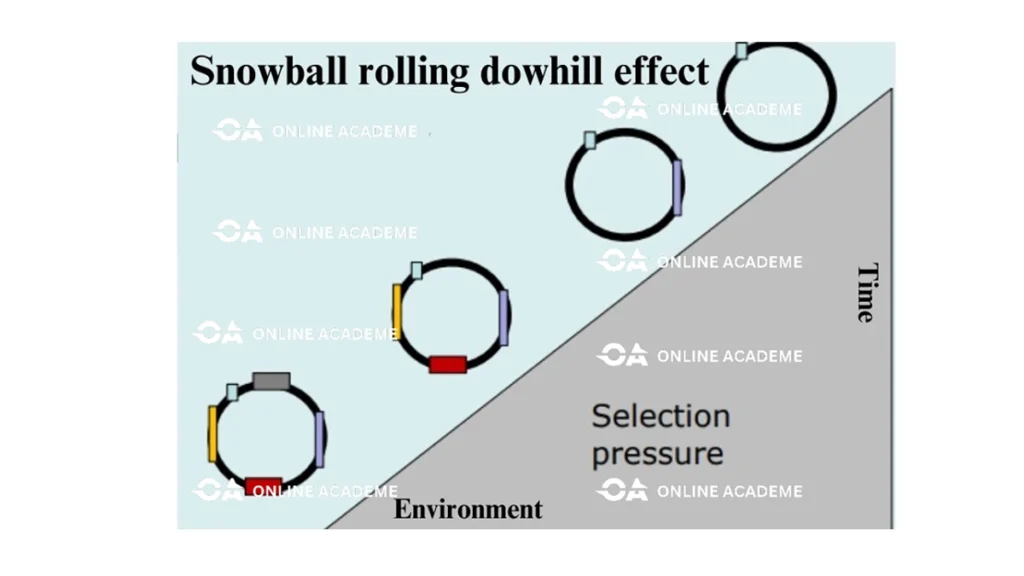
“Antibiotic selection pressure exerts “Snowball rolling downhill effect” in a bacterial population contributing to increasingly emerging antibiotic resistance”.
What is Antibiotic Selection Pressure?
Bacterial cells have inherent ability to develop resistance mechanism gradually against any chemical or drug which is continuously exposed to bacteria and this phenomenon is called selection pressure. Bacterial cells in the presence of antibiotic develop mechanisms to survive in their presence so that the antibiotic become ineffective with the passage of time through mutation or acquisition of resistance genes due to antibiotic selection pressure.
How Antibiotic Selection Pressure can be Addressed?
Antimicrobial resistance is a natural process however; human activities like overuse and misuse of antimicrobials are contributing significantly in accelerated development of antimicrobial resistance. Antimicrobial resistance can be addressed by a comprehensive approach that includes
- Prudent and judicial use of antimicrobial drugs
- Strict compliance with heightened infection prevention and control measures
- Monitoring of antibiotic resistance patterns through surveillance systems and
- Discovery of new antimicrobial drugs through research and development.

What is the theory of natural selection?
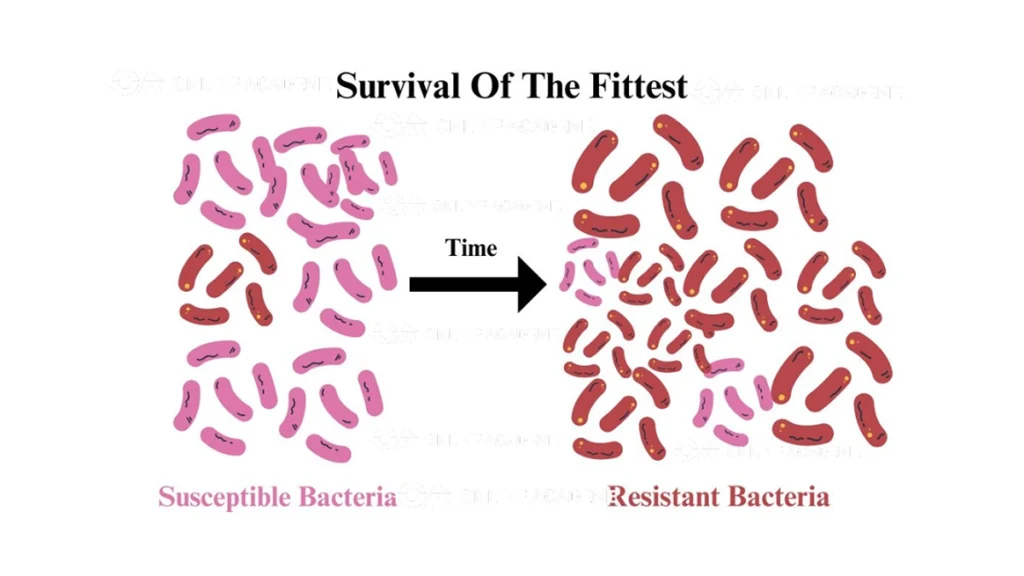
In 1859 Charles Darwin “Survival of the fittest” proposed his theory of evolutionary selection which explains how a specie or organism survives or get extinct due to its ability to adapt to change in the environment that may occurs randomly or may be induced. This theory is also called theory of natural selection. Antibiotic selection pressure plays a vital role in the emergence and spread of antibiotic resistance in bacteria.
What is antibiotic exposure and how it is induced?
Continuous misuse and overuse of antibiotics in an environment (human hospitals, livestock farms or agriculture land) for clinical use (to treat infections) or prophylactic use (to avoid infections), expose bacteria to antibiotics, the drugs target and kill susceptible bacteria. However, few bacteria may have natural variations or mutations in their genetic material that provide them with a survival advantage against that antibiotic. In addition to this, these bacteria will gradually adopt resistance genes to survive in high antibiotic concentration environment leading to highly resistant bacterial species.
Why few bacteria are not susceptible in bacterial population?
This may be due to the phenomenon called “Genetic Variation”. There is natural genetic diversity due to random mutations and genetic recombination within a bacterial population which leads to differences in antibiotic susceptibility pattern of different bacteria in a population. Due to genetic variation, few bacteria in a bacterial population may possess pre-existing resistance mechanisms. Therefore, most bacteria are killed by the antibiotic but a small proportion may possess genetic traits due to genetic variation that make them resistant to the antibiotic.
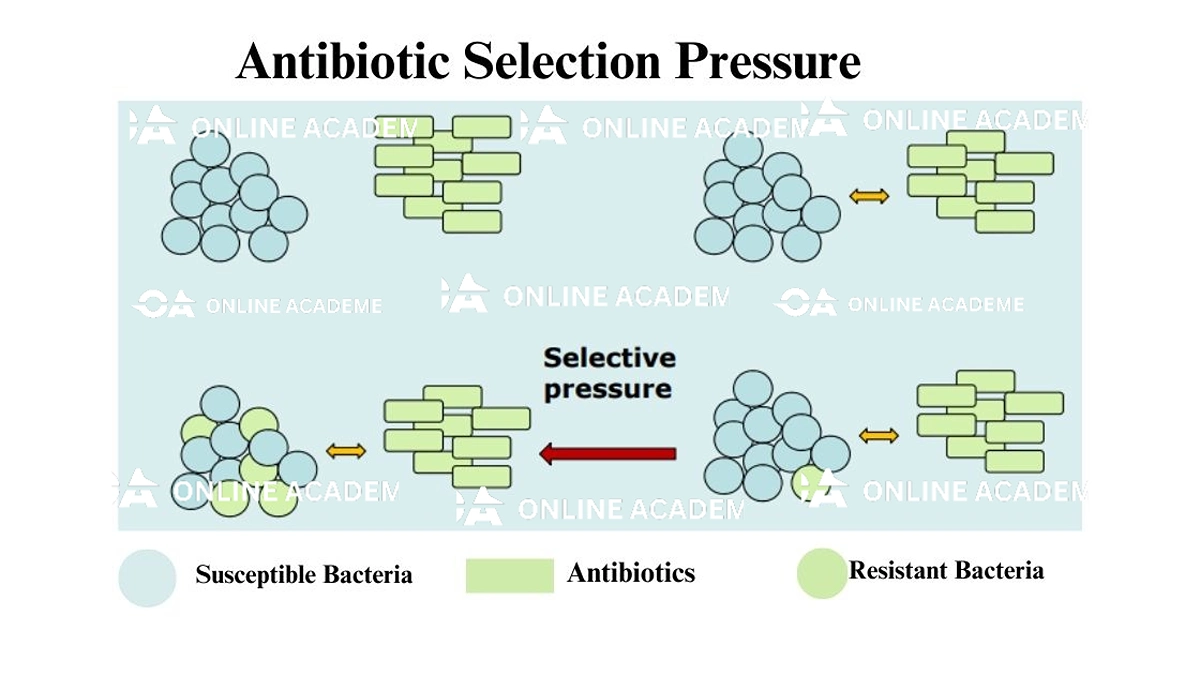
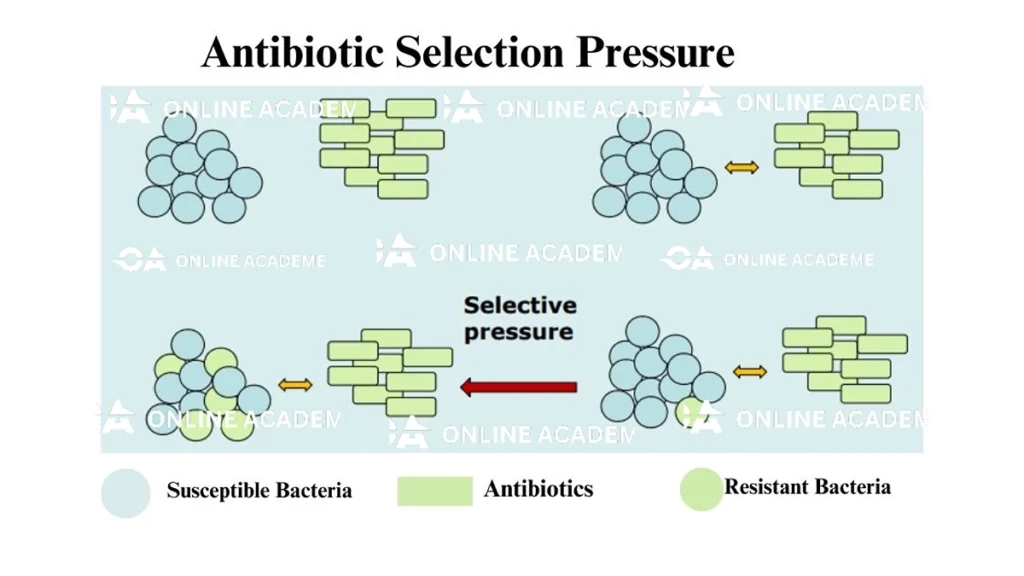
How antibiotic selection pressure induce antibiotic resistance?
Antibiotic presence in an environment induces selective pressure on the bacterial population within that environment due to continuous exposure. As a result susceptible bacteria are killed due to antibiotic which may include beneficial bacteria or normal microflora along with pathogenic target bacteria. However, there are few bacteria which may have genetic mutation and they survive antibiotic exposure.
The bacteria which survive and acquire resistance genes may be beneficial bacteria, normal flora or environmental bacteria along with pathogenic target bacteria. The resistant bacteria have a survival advantage and can multiply. This selective advantage allows the resistant bacteria to become more prevalent in the population over time by multiplication. Moreover, these bacteria further spread and disseminate resistance genes to other bacteria as well.
How selection pressure contribute in spread of antimicrobial resistance?
Resistant bacteria emerged as a result of antibiotic selection pressure acquire antibiotic resistance genes in their genetic material (chromosome or plasmid). These resistant bacteria transfer genetic material carrying antibiotic resistance genes to other bacteria through vertical or horizontal mechanism of gene transfer for example binary fission, conjugation, transformation, and transduction.
Horizontal gene transfer may be among different bacterial species i.e. transfer of antibiotic resistance genes between beneficial (normal flora) and pathogenic bacteria causing serious diseases, making disease causing bacteria resistant further promoting the development and dissemination of antimicrobial resistance.
How selection pressure make bacterial specie completely resistant?
Bacterial population gradually emerge as completely resistant to the antibiotic over successive generations due to the survival and proliferation of antibiotic resistant strains under antibiotic selection pressure. As a result of this evolution and spread, antibiotic resistant bacteria can multiply and potentially cause deadly infections which are difficult to treat.
How multi-drug resistant bacteria emerge due to antibiotic selection pressure?
Multidrug resistant bacteria are bacteria who are resistant to at least three classes of antibiotics. Multidrug resistant bacteria may emerge due to
- Repeated cycles of exposure by different classes of antibiotics.
- Natural selection and adaptation which may lead to evolution and emergence of multidrug-resistant bacteria
- Spread and dissemination of antibiotic resistance genes carrying genes against multiple drugs.
Emergence of multidrug resistant bacteria makes infections more challenging to treat.
What are driving factors which develop antibiotic selection pressure?
Overuse and misuse of antimicrobials
The overuse and misuse of antimicrobial drugs is the major factor which accelerate the emergence of antimicrobial resistance. Inappropriate use of antimicrobials like
- Prescription of antibiotics for viral infections e.g. monkeypox, covid-19
- Under dose of prescribed antibiotics (e.g., incomplete courses of antibiotics)
- Use of antibiotics as prophylactic measure ( e.g. use of antibiotics in poultry feed)
- Overuse of antibiotics without prescription (self-medication)
These practices create an environment which puts pressure on bacterial population that favors the survival and proliferation of resistant microorganisms. As a result of evolution and adoption resistance bacteria emerge due to antibiotic selection pressure.
Transfer between different reservoirs:
Antibiotic resistance genes through mobile genetic elements may be transferred between different reservoirs of microorganisms, including humans, animals, agriculture and the environment irrelevant of the bacterial specie. Antibiotic resistant bacteria also transfer between humans and animals through close contact or the consumption of contaminated animal food. Moreover, antibiotic resistant genes acquired by normal flora or beneficial bacteria can also be transferred to pathogenic bacteria which can cause emergence of antibiotic resistance in pathogenic bacteria. Additionally, the release of antimicrobial residues into the environment, such as through wastewater, can contribute to the spread of antibiotic resistance genes among different reservoirs (i.e. human, animal and agriculture).